The “Bernese periacetabular osteotomy” (PAO) was developed by Professor Reinhold Ganz and his colleagues in Switzerland. PAO surgery is most commonly used to treat acetabular dysplasia or a “shallow hip socket” (human hip dysplasia). Dr. Clohisy commonly performs PAO surgeries in St. Louis, and many of our research studies are focused on improving the care of patients with hip dysplasia. Below, we introduce the basic concepts of hip dysplasia, secondary osteoarthritis, and the surgical treatment of this disorder.
Human Hip Dysplasia, Acetabular Dysplasia
In a “normal” hip, the head (ball) of the femur (thigh bone) is covered adequately and well seated in the acetabulum (hip socket). The hip socket is “cup shaped.” In contrast, a dysplastic hip has incomplete or inadequate coverage of the femoral head. The dysplastic hip is more “dish shaped.”
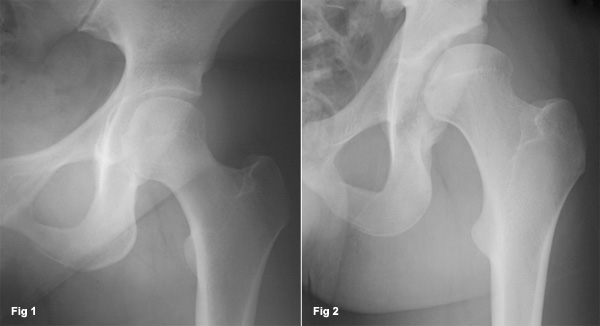
Fig 1. Normal Hip: Normal ball and socket hip joint with a well-seated femoral head (ball) and normal acetabulum (socket); Fig. 2 Dysplastic Hip: A dysplastic hip with a shallow hip socket and partial femoral head coverage.
Because of the inadequate coverage of the femoral head in a dysplastic hip, the weight across the hip is distributed on a smaller surface area resulting in excessive load along the rim of the hip socket. Over time, this increased load along the rim of the socket will lead to degeneration of joint cartilage and formation of osteoarthritis. Patients with this condition frequently seek medical attention due to activity-related hip pain (discomfort in the groin or side of the hip). Prolonged sitting or walking can also increase these symptoms and a sensation of catching or popping may also occur. As these symptoms continue to increase, a slight limp may be noticed and more strenuous activities may become difficult.
Diagnosis of Acetabular Dysplasia
The diagnosis of symptomatic hip dysplasia is made by a complete medical history, physical examination, and an x-ray evaluation. An x-ray is taken to assess for a hip joint deformity and secondary osteoarthritis. Some patients may have been treated for hip problems as an infant or child. Nevertheless, symptoms may develop if there is a residual deformity, even if the patient had previous treatment. With this information, Dr. Clohisy may recommend surgical treatment to correct the hip deformity. Our treatment of choice for this condition is called a periacetabular osteotomy (PAO).
Periacetabular Osteotomy (PAO)
PAO surgery is a hip preservation surgery performed to correct a congenital or developmental deformity of the acetabulum known as acetabular dysplasia. If this condition remains untreated, secondary arthritis commonly develops. Therefore, in order to relieve symptoms and improve the prognosis of the hip, this surgery is done to correct the bony anatomy and help normalize the load across the joint.
“Periacetabular” means around the acetabulum (hip socket). “Osteotomy” means to cut bone. Therefore, PAO means to cut the bone around the acetabulum and reposition the hip socket. The PAO is a very effective procedure for the treatment of symptomatic acetabular dysplasia. Dr. Clohisy, his colleagues and healthcare team have an extensive experience in the evaluation and treatment of patients with hip dysplasia.
At surgery, controlled cuts are made to loosen the acetabulum from the pelvis, and the acetabulum is repositioned. An incision is made across the front of the hip joint to allow exposure of the hip and surrounding pelvis. The use of x-ray during surgery helps direct the bony cuts and confirm the correct reorientation of the socket. The acetabulum is fixed in the new position with three or four screws. In most uncomplicated cases the surgery takes two to three hours.
Video: PAO Surgery for Acetabular Dysplasia
An educational video showing periacetabular osteotomy, how PAO surgery works and when PAO is used, as well as some risks and benefits of the PAO procedure.

A pelvic model is shown and demonstrates the bony cuts and repositioning of the acetabulum. The gaps between the repositioned bone fill in with new bone, just like the healing of a fracture.

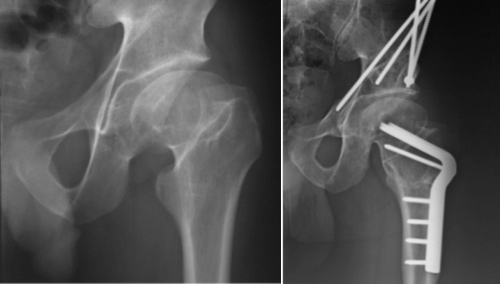
X-rays of a 25-year-old female with bilateral hip dysplasia are shown (top panel). This patient was treated with PAOs and she has an excellent result in both hips five years after her PAO surgery (bottom panel).
Occasionally (approximately 1 out of 20 cases) there is also a deformity of the femur that must be corrected at the time of surgery by a proximal femoral osteotomy (PFO). This involves cutting and repositioning the upper portion of the femur bone. If this is indicated, a second incision is made along the outside of the hip and the femur is repositioned and fixed with a metal plate and screws.
Preoperative x-rays of a 19-year-old male with deformity of the hip socket and femur secondary to Perthe’s Disease (left). Four years after surgery with the correction of the acetabulum and femur, this patient has no hip pain and an excellent result from surgery (right).
The hospitalization time is two to four days and full recovery takes four to six months. The majority of patients experience major relief of pain and become quite active after recovery from surgery. While the PAO is an extremely effective hip preservation procedure, it may not create a completely normal hip. Even if the PAO is effective in adolescence or early adulthood, some patients are likely to require a total hip replacement surgery later in life.
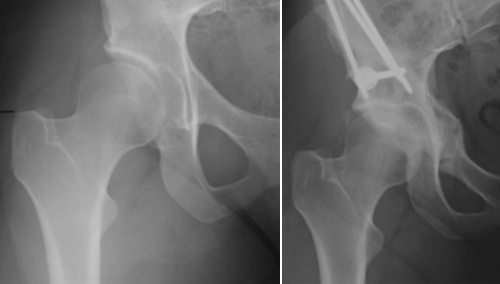
19-year-old female soccer player with right hip pain and acetabular dysplasia (left). Five years after PAO surgery. The patient reports no pain and has returned to full activities. Note improvement of femoral head coverage (right).
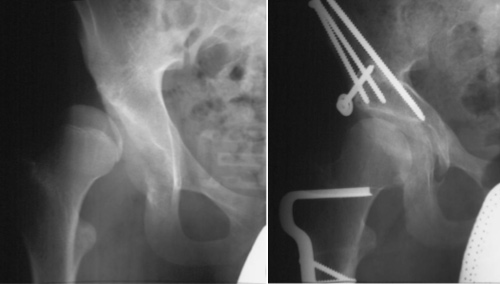
15 year-old male with right hip pain and severe dysplasia (left). Nine years after PAO surgery. The patient was treated with a PAO and PFO. He reports no pain and has returned to full activities (right).
Many patients with hip dysplasia (shallow socket) have other problems within the joint (cartilage tears) and/or may have a deformity of the femoral head of femur bone. Commonly, these other problems are treated during the PAO procedure. Hip arthroscopy may be used to treat problems within the joint while reshaping of the femoral head is also commonly performed at the time of the PAO.
Rehabilitation from PAO Surgery
After a PAO, patients are usually on crutches for four weeks with “touchdown weight bearing.” A continuous passive motion (CPM) machine is used to assist joint healing. We then advance weight bearing as tolerated at four weeks, and anticipate unassisted walking at six to eight weeks. Strengthening exercises and nonimpact activities (cycling, swimming, elliptical) are also progressed at four weeks. For athletes, jogging starts three months after surgery and return to full sport is allowed at four months.

CPM machine to promote joint healing and relieve stiffness.
Risks, Complications with PAO Surgery
Like all surgeries, the PAO has some risk of complications. The overall complication risk is low in the hands of experienced surgeons. Potential complications include, but are not limited to, nerve or artery injuries, fractures, infection, blood clot formation, non-union of the bone, persistent hip pain, and osteoarthritis progression.
More on Acetabular Dysplasia and Periacetabular Osteotomy
Periacetabular osteotomy (PAO) surgery may be the right treatment option for your acetabular hip dysplasia. An experienced PAO surgeon based in St. Louis, Dr. Clohisy will assess your hip dysplasia and help you decide on treatment. For more information on acetabular dysplasia and periacetabular osteotomy (PAO) surgery, try these sources: