Perthes Disease is a hip disorder in which a portion of the ball-shaped head (femoral head) of the thigh bone (femur) loses blood supply and dies. The femur or thigh bone has a ball-shaped end that fits into the hip socket to create a ball-in-socket joint. In a healthy individual, the bones of the body, including the femoral head, are nourished by oxygen-rich blood. If something disrupts the blood supply to the femoral head, the bone dies. The femoral head can become soft and misshapen during this disease process. This can lead to hip pain and subsequent hip arthritis.
Perthes Disease is characterized by four main stages, which occur in this order:
| Phase | Medical Name | What Happens | Length |
| 1 | Necrosis | A portion of the femoral head dies. This changes the shape of the femoral head and can cause pain, stiffness, and inflammation. | Up to 1 year |
| 2 | Fragmentation | The dead cells are absorbed by the body and can be replaced by new, healthy bone cells. As the new femoral head is formed, it is “remodeled” producing varying femoral head shapes. | 1-3 years |
| 3 | Reossification | The femoral head continues to grow with new bone cells. | 1-3 years |
| 4 | Remodeling | The new bones cells are gradually replaced by normal bone cells, and remodeling continues. | 1-3 years or more |
Other Names of Perthes Disease
Perthes Disease is also called Legg-Calve-Perthes Disease, LCPD, ischemic necrosis of the hip, coxa plana, osteochondritis, and avascular necrosis of the femoral head. It is a form of osteonecrosis, and literally means “bone death.”
Causes of Perthes Disease
The underlying cause of Perthes Disease is not known. The various processes that occur in Perthes Disease are caused by an interruption of blood supply to the femoral head. With our present state of medical knowledge, Perthes Disease cannot be prevented.
Symptoms
Parents typically first notice that the child walks with a limp or complains of pain in the hip or groin. In some cases the pain occurs in other areas of the body (a phenomenon called “referred pain”) such as the knee. There may be limited mobility of the hip. When questioned by parents, the child usually cannot remember injuring the hip. Pain may be insignificant or absent in some patients with Perthes disease.
Diagnosis
Any complaints of persistent hip pain should be evaluated by an orthopaedic surgeon. The evaluation should include a medical history, physical examination and x-rays of the hip. An MRI of the hip is also a common part of the hip evaluation.
Defining the Condition
Physicians use certain classification systems to help describe the progress of Perthes Disease. These classification systems analyze the extent of bone involvement, the location of the diseased bone and the shape of the femoral head and acetabulum. These characteristics of the hip assist in making an effective treatment plan. Children with Perthes Disease should be evaluated and treated by a pediatric orthopaedic surgeon. Adolescents and young adults with residual hip deformities from Perthes Disease should be evaluated by an orthopaedic surgeon with interest in joint preservation hip surgery. Dr. Clohisy has a specific interest in patients with residual Perthes deformities.

Radiograph of the right hip in a patient with residual Perthes deformities. The deformity includes a shallow and inclined acetabulum (hip socket), an elliptical femoral head, short neck and high trochanter. Many patients with this type of deformity experience pain and/or develop osteoarthritis at a young age.
Treatment
Patients with Perthes Disease may present for treatment in childhood with active disease or may present for treatment after skeletal maturity with residual Perthes Disease. In children, the goal of treatment is to make the resolution of the condition as speedy, painless, and successful as possible. If the remodeling of the femoral head is imperfect, patients are at risk of degenerative arthritis later in life. The results of treatment for Perthes are quite variable and largely depend upon the condition of the femoral head when the patient firsts consults with the physician. Active Perthes Disease in childhood is best managed by a pediatric orthopaedic surgeon.
There are some typical nonsurgical treatments for Perthes Disease:
- Physiotherapy in order to maintain good range of motion
- Crutches to limit the weight on the hip joint
- Braces, casts, or traction may be required
In some instances, surgery may be appropriate. However, Dr. Clohisy does not treat Perthes Disease in young children. Surgical options (soft tissue releases, osteotomies and others) are best described by a pediatric orthopaedic surgeon.
Residual Perthes Deformities
Many patients seek care in adolescence or young adulthood (10-40 years) with hip problems from “residual” Perthes disease. These patients had Perthes during childhood producing a hip deformity that becomes problematic years later. These hips can have a variety of problems including a misshapen femoral head, short femoral neck, high greater trochanter, and a shallow hip socket. The hip may also have cartilage tears and/or arthritis. Treatment of these residual deformities is difficult and may include a surgical hip dislocation and/or a hip osteotomy. These procedures are outlined in other areas of the website. Joint preservation surgery to treat Perthes Disease is targeted at correcting the hip deformity, relieving pain, increasing activity and preserving the natural hip joint. Occasionally, the hip will be too arthritic for joint preservation surgery and a total hip replacement may have to be considered.
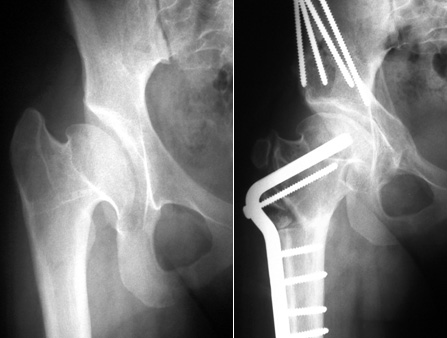
X-rays of a 13-year-old girl with severe Perthes deformity showing treatment of the femoral head by reshaping and osteotomies of the acetabulum and femur. This patient had an excellent clinical result 4 years after surgery.
Perthes Disease Facts and Figures
- Active Perthes Disease only occurs in children (but residual deformity can cause problems in adolescents and adults)
- About 75% of children affected by Perthes Disease are boys
- About 95% of children with Perthes Disease will have it in only one hip
- The average age at diagnosis is 6 years
- Perthes Disease is more common among Asians, whites, and Eskimos and less common among blacks, Native Americans, and Polynesians
(Statistics from National Osteonecrosis Foundation.)